Overtaxed Idaho health facilities on brink of rationing care
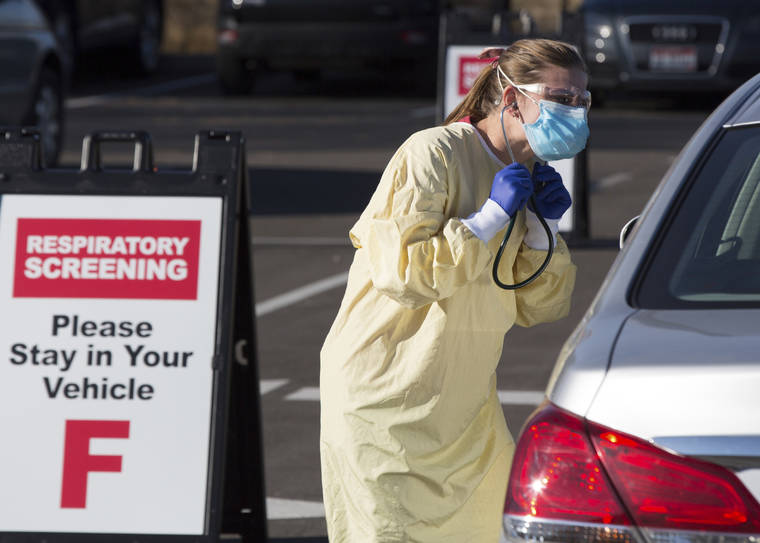
Physician assistant Nicole Thomas conducts a COVID-19 examination in the parking lot at Primary Health Medical Group’s clinic in Boise, Idaho, Tuesday, Nov. 24, 2020. The urgent-care clinic revamped into a facility for coronavirus patients as infections and deaths surge in Idaho and nationwide. Some 1,000 people have died due to COVID-19, and infections this week surpassed 100,000. (AP Photo/Otto Kitsinger)
BOISE, Idaho — Soldiers triaging patients in parking lots in a capital city is normally the stuff of science fiction.
BOISE, Idaho — Soldiers triaging patients in parking lots in a capital city is normally the stuff of science fiction.
Yet that’s the reality in Boise, where troops direct people outside an urgent-care clinic revamped into a facility for coronavirus patients as infections and deaths surge in Idaho and nationwide.
Inside Primary Health Medical Group’s clinic, physician assistant Nicole Thomas works extra 12-hour shifts to help out. She dons goggles, an N95 mask, a surgical mask over that, gloves and a body covering to examine 36 patients a day with symptoms. Some days, she says, half of them test positive for COVID-19.
“I’ve had patients crying in the car because they think they’re going to die,” Thomas said last week, resting against a desk between patients. “There are some people that it’s just a mild cold, and there are some people in the ICU on life support. We don’t know, medicine-wise, how it’s going to affect them.”
What was once a facility with family practice doctors and an urgent care that treated things like cuts and colds has become a COVID-19 clinic, showing how a crush of virus patients is straining intertwined health care systems. In a conservative state where many are resisting pandemic restrictions, overworked staff are getting sick themselves or quitting to avoid the stress.
Idaho’s attempt to hold the coronavirus in check is failing, health officials say. Just over 1,000 people have died from COVID-19 so far, about four to five times the number of annual deaths from flu and pneumonia. Confirmed infections have surpassed 100,000.
Elective surgeries mostly have been halted to conserve bed space and staff. COVID-19 patients have been sent home with monitoring devices to care for themselves. After Thanksgiving gatherings, officials fear a surge of infections that could force difficult choices about what to do with patients when there’s no more room or anyone available to treat them.
“When would we reach absolute capacity? I just don’t know. But we’re nervous,” said Barton Hill, vice president of St. Luke’s Health System, which has hospitals in southwestern and central Idaho.
“I never dreamed that we would be challenged like this,” Steve Judy, chief operating officer of Primary Health Medical Group, said as he visited the clinic where Thomas works.
He was interrupted by a young woman there for a COVID-19 test who wandered out of an exam area, looking confused. She had blood drawn and wasn’t sure where she was supposed to be, she said through her mask, eyes glazed. Judy, after determining her checkup wasn’t done, gently led her past a row of workers taking phone calls and back to the exam area.
The clinic bustled with workers, supporting Thomas and two other physician assistants who examine patients. Combined, they see nearly 110 people a day, ordering chest X-rays and blood tests to make a diagnosis. Seventy others without symptoms get drive-thru COVID-19 tests in the parking lot every day.
Primary Health’s 20 clinics in southwestern Idaho normally have an urgent care on one side and family practice doctors on the other. Eight have been transformed into facilities that only see COVID-19 patients.
It’s taking sick people at least two days to get an appointment for a test. Primary Health will turn three more facilities into COVID-19 clinics by Dec. 30 and has plans to change over more if needed.
“I’m not at the hospitals,” said Dr. David Peterman, a pediatrician and CEO of Primary Health Medical Group. “But I’m telling you, we’re at the maximum at Primary Health. We are so close to rationing care here. We are probably 10 to 15 days away.”
About 20% of his staffers are out because they’re isolating or have tested positive for the virus. Judy said he’s trying to fill 50 openings after workers couldn’t take the stress anymore and quit. He’s increased front office pay by $2.50, to $14 an hour.
Calls to the clinics have increased from 30,000 a month before the pandemic to 80,000 now. The Boise clinic has a half-dozen workers taking calls. When they’re not on the phone, they package test kits.
“We’re working them hard,” said Judy, who worries about his staff. “They’re almost all pulling overtime.”
At St. Luke’s hospital system, increasing numbers of workers are out because of COVID-19, officials said. Besides canceling elective surgeries, the hospitals tried to save bed space by sending 160 patients — 140 with COVID-19 — home with devices to measure the oxygen in their blood.
Now, hospitals are planning what to do if there aren’t enough workers or beds available in an entire region. Health care workers would have to choose who gets treatment and who doesn’t.
“That’s really when we’re at risk for what’s called the ‘crisis standards,’” said Hill, noting that the state would decide when to institute them. “We’re very concerned in the next two weeks.”
Idaho’s crisis plan divides the sick into categories, prioritizing those with life-threatening illnesses or injuries who are expected to survive and giving only comfort care to those who aren’t.
Rural areas generally avoided large numbers of COVID-19 infections for months but now they’re widespread. Recently, a surge of infections in southern Idaho filled hospital beds and forced some patients to be transferred to the Boise area.
When people started getting sick in March, Republican Gov. Brad Little issued a stay-at-home order that lasted just over a month and stopped the virus’s spread. But unemployment skyrocketed from under 3% to nearly 12%.
Restrictions gradually were lifted, but as infections and deaths surged again, Little reinstated some rules last month, including limiting gatherings to 10 or fewer. He also activated 100 National Guard troops to free up medical workers, getting them trained on mobile testing support, facility decontamination and COVID-19 screenings.
Nickolas Orr was one of two soldiers meeting patients in their cars outside the Primary Health clinic.
“Some people do seem a little nervous,” he said, directing them where to go depending on whether they were sick and had an appointment or felt fine but wanted a test.
While Little was among the first governors to publicly wear a mask last spring, he’s declined to issue a statewide mandate, saying more people will wear them if it’s a choice.
There’s plenty of resistance. About 64% of Idaho voters supported President Donald Trump, who has been dismissive of mask-wearing and ridiculed President-elect Joe Biden for wearing one during the campaign.
Some sheriffs say they won’t enforce mask requirements. A lawmaker has compared Little to Hitler for issuing pandemic restrictions. The Republican-dominated Legislature plans legislation next month limiting the governor’s ability to declare emergencies.
And in Boise, which has a mask mandate, protesters recently went into stores and restaurants without face coverings to complain that their rights were being violated.
Meanwhile, inside the Primary Health clinic, Thomas, the physician assistant, put on sterilized protective equipment as workers sanitized an exam room before the next patient.
The clinic no longer has time to call everyone who tests positive for COVID-19. Most get a text. Only those in high-risk groups with the greatest chance of dying get a phone call, that human voice.
“Not infecting others is kind of the name of the game right now,” Thomas said. But she doesn’t have a lot of hope. “I think we are going to get busier and busier.”