A soft tissue infection more commonly known as flesh-eating bacteria has now been diagnosed in three unrelated cases on Kaua‘i.
Janice Okubo, communications director for the Hawai‘i Department of Health, said on Monday that three cases of the rare, but sometimes deadly infection called necrotizing fasciitis have been reported to the department.
“The third case, which previously had not yet been diagnosed as necrotizing fasciitis, has since been deemed as clinically compatible with NF by the attending physician,” Okubo said.
A Lihu‘e woman whose adult son remains hospitalized and undergoing a series of surgeries for flesh-eating bacteria said Monday that people should be careful to avoid contact with dangerous bacteria when they have scratches or cuts.
Janice Bond said her son, John Stem, 49, of Lihu‘e, probably contracted it climbing in and out of crawl spaces and attics as part of his job as a sales agent for a pest control company and infecting an existing scratch. Stem is believed to have scratched his leg below the knee on a “thorny bush,” Bond said.
“I just want people to be aware that if they have any redness, or any soreness, to seek treatment,” she said after returning from O‘ahu, where her son remains hospitalized.
Necrotizing fasciitis is caused by Group A streptococcus, a form of bacteria that can destroy skin tissue.
“I was told Strep A is everywhere,” she said, adding that she is especially worried about crews working to repair roads on the island in the wake of recent heavy rains and flooding.
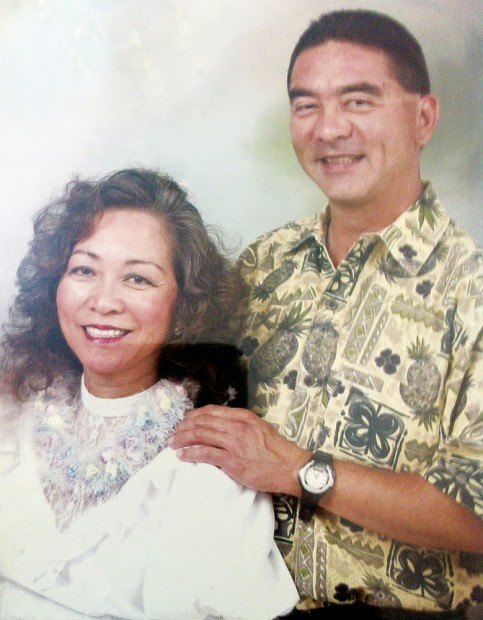
Stem already has endured several surgical procedures to remove dead flesh from his thighs and back, and was suffering from secondary infections Monday, Bond said. She carried a picture of her son showing strips of skin had been removed from his thigh.
“It’s not over,” Bond said. “It’s going to be very costly, but he’s alive.”
Bond found her son unconscious in his home on March 10, and he was transported to Wilcox Memorial Hospital in Lihu‘e.
“The doctors at Wilcox were instrumental in saving his life,” she said.
Following several surgeries, he was transferred to a hospital in O‘ahu to continue treatment at the Kuakini Medical Center in Honolulu.
Stem will be treated at the Hyperbaric Treatment Center on the hospital campus, his mother said. The center is part of the University of Hawai‘i John A. Burns School of Medicine. Hyperbaric medicine is used to promote the healing of damaged skin tissues.
Joe Elm, a biologist and epidemiological specialist with the state Department of Health, said the Center for Disease Control tracks the invasive Strep A bacteria-related illnesses nationwide. He said that of about 10,000 cases annually, only about 6 percent meet the criteria of this syndrome.
The syndrome itself has a damage spectrum ranging from seemingly normal to severe. The syndrome presents no identifying or underlying cause about 3 percent of the time, Elm said. These are the rare cases, including the three this week on Kaua‘i.
Necrotizing fasciitis is typically identified as Type 1 multiple bacteria and Type 2 single bacteria, Elm said.
The Kaua‘i victims differ in that one acquired it from a single bacteria, the second from multiple bacteria, and the third from a Strep and mixed bacteria infection.
When it comes to prevention, “clearly, attention to wound care is the most important issue,” Elm said.
People will wash a wound and put a bandage on it and forget about it, he said, but it is important to keep a wound clean and to see a physician if they experience fever, pain and other warning signs that healing is not occurring.
Bacteria can enter skin through a small coral cut in clean ocean water as easily as it can in dirty flood water, Elm said. These bacteria are on the skin, and it would not take much trauma to get underneath and do damage.
The bacteria might cause Strep throat in one person and leave another with no symptoms, he said.
Elm said the concern is getting people to care for wounds, practice good hygiene and wash hands thoroughly to reduce colds and flu and food-borne diseases.
The syndrome was first described in the Civil War when it took a long time to get soldiers adequate care. Elm said war trauma to the skin is severe, and the delay in treatment allowed bacteria to push under the skin.